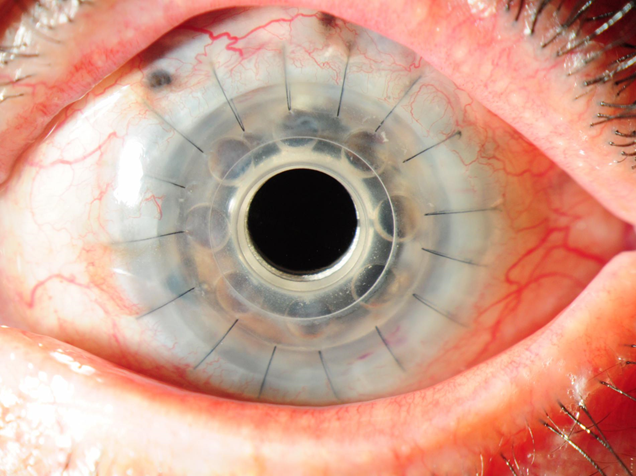
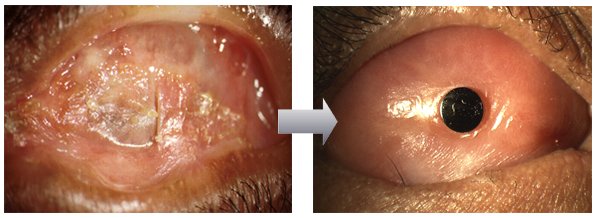
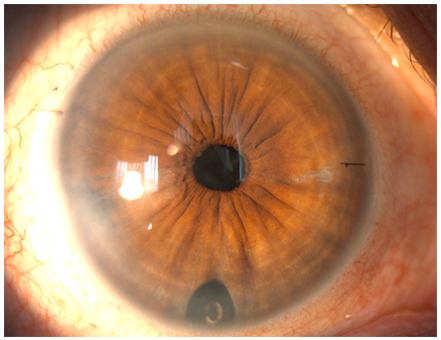
The Cornea consists of several layers, and in many patients, not all the layers are diseased or damaged. In the past, corneal surgeons only performed one main procedure – the Penetrating Keratoplasty (PK) operation, whereby the entire central aspect of the cornea was replaced by a donor cornea – a full-thickness transplant.
Penetrating Keratoplasty
Today, several forms of corneal transplantation procedures exist, and it is now possible to selectively replace different layers of the cornea, whilst retaining the unaffected layers. The major advantages to just replacing the diseased layers, and leaving the healthy layers untouched, include a stronger eye after surgery, good visual quality, relatively quick visual recovery, and most importantly, a marked reduction in complications, both during and after surgery, which leads to good success rate overall. These forms of partial thickness corneal transplantation are termed Lamellar Keratoplasty procedures.
There are basically 2 forms of modern Lamellar Keratoplasty:
- Anterior Lamellar Keratoplasty (ALK)
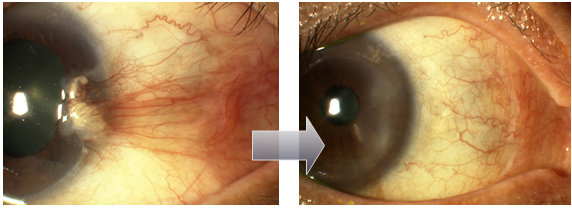
ALK procedures involve exchanging only the front layers of the cornea, leaving the innermost layer (the Endothelial Layer), intact and unchanged. The commonest ALK procedure today is Deep Anterior Lamellar Keratoplasty (DALK), where all the front layers of the cornea are fully exchanged. The major advantage of DALK is that the risk of corneal transplant rejection is reduced to a 1-2% risk, compared to PK surgery, where the risk of rejection may be as high as 10-15%. With a DALK procedure, it is also often possible to achieve the good visual quality, and because the risk of rejection is much less, less anti-rejection steroid eyedrops are used after surgery, which also means a reduction in other complications such as glaucoma, and infection.
- Endothelial Keratoplasty (EK)
In many instances, corneal clouding is due to an ageing or abnormal innermost layer of the cornea, known as the Endothelial Layer, which consists of Endothelial Cells which are either insufficient in numbers or are damaged. EK procedures leave the front layers of the cornea intact, and instead just exchange the innermost layers which contain the endothelial cells needed to keep the cornea clear. Because the donor endothelial layer is usually inserted through as small side incision (similar to “keyhole surgery”), there are no sutures on the cornea (“sutureless surgery), and vision recovers much at an earlier rate than PK or ALK. EK is usually performed as a Day Surgery procedure, and can also be performed under Local Anesthesia (LA)(just an anesthetic injection around the eye), as opposed to a full General Anesthesia (GA). The risk of transplant rejection is also much lower than PK, and ranges from 1-4%.
There are 2 forms of EK surgery, DSAEK (Descemets Stripping Automated Endothelial Keratoplasty), and DMEK (Descemets Membrane Endothelial Keratoplasty).
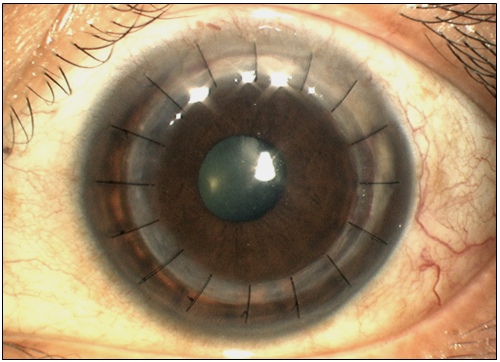
In DSAEK, a slightly thicker layer of inner corneal tissue, consisting of several layers, is transplanted – this procedure has been shown to have good vision restoration, less complications – rejection as compared to PK, in the region of 2-4%, and is therefore a relatively common form of transplantation in the West and in advanced countries.
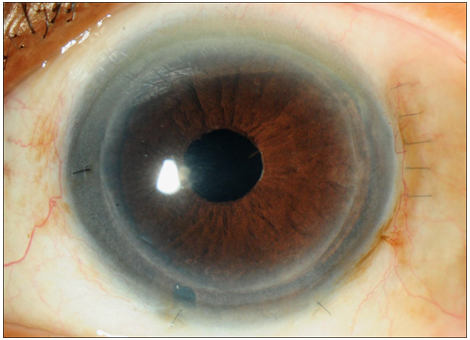
Descemets Stripping Automated Endothelial KeratoplastyDMEK is a relatively later version of EK surgery in which only the innermost membrane and the endothelial cells are transplanted – this thin and delicate layer makes the surgery more challenging, and only a few surgeons perform this procedure at present, but the main advantages of DMEK is that the rejection rate is only about 1%, and DMEK offers good quality vision after surgery.
Descemets Membrane Endothelial KeratoplastyIn both DSAEK and DMEK, repeat corneal transplantation can be more easily performed, as compared to PK surgery, and can also be combined with other forms of surgery such as cataract removal and intraocular lens implantation at the same sitting.
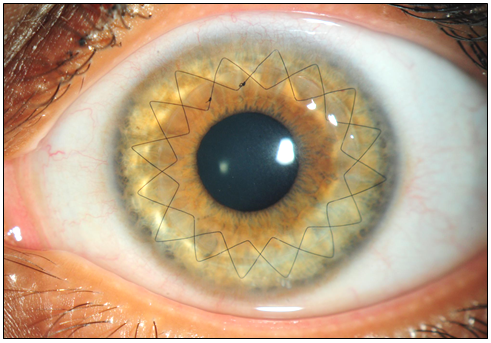
Deep Anterior Lamellar Keratoplasty